How Third-Party Administrators (TPAs) Enhance Self-Funded Health Plans

As the healthcare environment continues to evolve, many employers are moving away from traditional fully-insured models to adopt self-funded health plans. In these plans, employers directly finance healthcare expenses, offering them more control and the potential for cost savings. However, this model also presents complex administrative challenges. To address these hurdles, employers are increasingly turning toThird-Party Administrators (TPAs) to streamline plan management. TPAs provide expertise and support, enabling employers to focus on the well-being of their workforce while navigating the complexities of self-funded health plans.
This article delves into the pivotal role TPAs play in enhancing self-funded health plans. By outsourcing essential tasks such as claims processing, compliance management, and more, TPAs help employers achieve greater efficiency, reduce costs, and improve employee satisfaction. This shift marks a move towards a healthcare model that emphasizes value over volume, as explored further on Health Compiler’s blog.
Understanding TPAs in Self-Funded Health Plans: A New Paradigm
In a self-funded health plan, the employer takes on the financial responsibility of covering employee healthcare claims directly. Unlike traditional insurance models, where premiums are paid to a third-party insurer, self-funded plans require employers to manage these expenses. This is where TPAs come into play. They offer specialized services to administer the plan, ensuring that employers can provide high-quality care without being bogged down by the administrative tasks that accompany healthcare management, as detailed byRoundstone Insurance.
TPAs assume responsibility for the operational backbone of self-funded plans, allowing employers to focus on their workforce's health and well-being. Let’s explore the key ways in which TPAs support self-funded health plans.
Key Ways TPAs Support Self-Funded Health Plans
Claims Processing Efficiency: TPAs handle the entire claims process, from submission to adjudication, ensuring that claims are processed in a timely and accurate manner. This not only reduces the administrative burden but also ensures that providers are paid promptly, keeping the plan running smoothly.
Learn more fromCollective Health
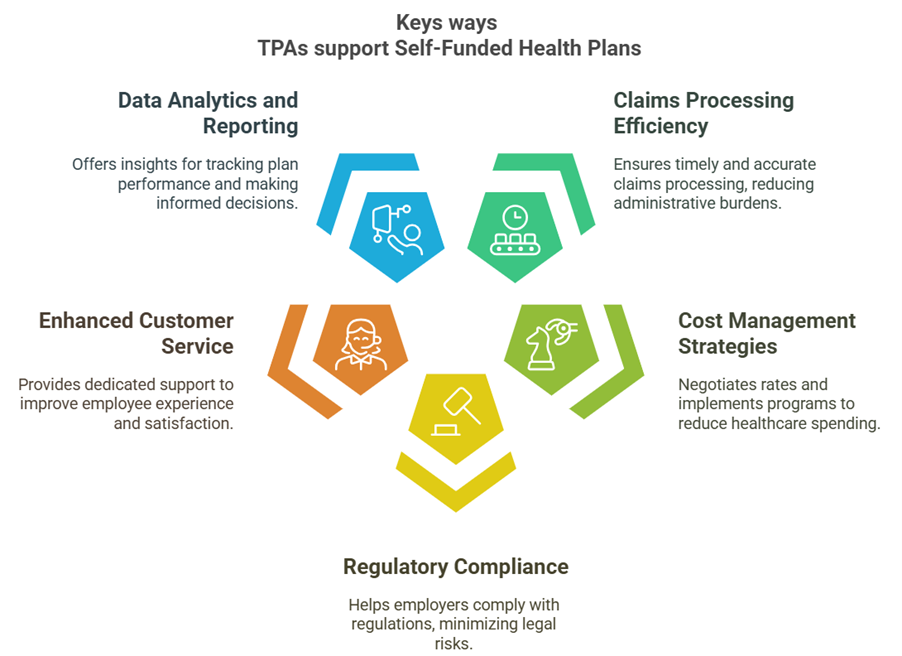
- Cost Management Strategies: By negotiating provider rates, implementing disease management programs, and using other cost-containment measures, TPAs help employers reduce their healthcare spending. These strategies can lead to significant savings while maintaining the quality of care for employees, as noted by6 Degrees Health.
- Regulatory Compliance: Self-funded health plans must comply with a range of regulations, including theEmployee Retirement Income Security Act (ERISA) and theAffordable Care Act (ACA). TPAs help ensure that employers remain compliant with these laws, minimizing legal risks and avoiding costly penalties, per insights fromTDI Texas.
- Enhanced Customer Service: TPAs offer dedicated support to employees, answering questions and resolving issues quickly. This enhances the overall employee experience and boosts satisfaction, which is crucial for maintaining employee engagement with the health plan, according toPersonify Health.
- Data Analytics and Reporting: TPAs provide valuable insights through health data analysis, helping employers track plan performance and make informed decisions. These analytics drive better outcomes, allowing employers to optimize their health plans over time, as explained byHealth In Tech.
- Chronic Condition Management: TPAs proactively monitor employees with chronic conditions such as diabetes, offering tailored care plans to reduce complications and long-term healthcare costs. This approach improves employee health while lowering the overall cost of care, a benefit highlighted byHNAS.
How TPA Support Differs from Traditional Insurance Models
Traditional insurance models tend to focus on volume, enrolling as many individuals as possible and processing claims in bulk. In contrast, TPAs focus on delivering high-quality, cost-effective care tailored to the specific needs of each employer. Here’s how TPAs differ from traditional insurance:
- Focus on Outcomes: TPAs prioritize achieving positive health outcomes for employees, which aligns with employers’ goals of promoting a healthier workforce as perVaripro.
- Sustainable Savings: Unlike traditional insurance models that may focus on short-term financial gains, TPAs aim for long-term cost control through prevention, efficiency, and wellness programs, as discussed byAssociation Health Plans.
- Personalized Administration: TPAs offer flexible, customized services to meet the unique needs of each employer, providing a level of personalization that traditional insurance models often lack.
- Proactive Health Strategies: TPAs emphasize prevention and early intervention, helping employees avoid costly emergency care and reducing overall healthcare expenses, a strategy endorsed byIPMG Blog.
- Innovative Measurement Approaches: TPAs use advanced metrics to assess the success of self-funded plans. They track accessibility, employer satisfaction, and comprehensive cost analysis to ensure that plans are achieving their goals.
Innovative Measurement Approaches: TPAs use advanced metrics to assess the success of self-funded plans
TPAs leverage cutting-edge tools to measure plan success beyond traditional metrics:
- Accessibility: Are employees getting timely care? TPAs evaluate this to ensure seamless access.
- Employer Satisfaction: Are plan goals met? Feedback loops refine TPA services.
- Cost Analysis: TPAs assess total plan performance, integrating wellness impacts, as seen inRoundstone’s insights.
Overcoming Obstacles in Leveraging TPAs
While TPAs offer numerous benefits, adopting a self-funded model with TPA support comes with its own challenges. Employers must navigate the paradigm shift from fully-insured to self-funded plans, which requires a change in mindset. Here are some common challenges and solutions for overcoming them:
- Paradigm Shift: Moving from a fully-insured model to a self-funded approach requires a shift in focus from volume to value. Employers must be willing to invest in the long-term success of the plan by prioritizing cost-effective care and employee health.
- Choosing the Right TPA: Not all TPAs are created equal. Employers must carefully vet potential TPAs for their expertise, technology capabilities, and track record in managing self-funded plans, as advised bySPBA TPA.
- Data Security: Protecting sensitive health data is paramount. TPAs must comply with privacy laws likeHIPAA and implement stringent data security measures to ensure that employees’ health information is kept safe.
Role of Technology in TPA Success
Technology plays a crucial role in amplifying the effectiveness of TPAs. Tools likeHealth Compiler and others are transforming the way TPAs manage self-funded health plans by providing real-time analytics, predictive monitoring, and seamless integration withElectronic Health Records (EHRs).
Key technological advantages include:
- Real-Time Analytics: TPAs can track claims and healthcare costs in real-time, enabling employers to adjust strategies quickly and proactively.
- Predictive Monitoring: TPAs can identify potential high-cost claims before they escalate, allowing employers to intervene early and manage expenses more effectively.
- Seamless Integration: By integrating with EHR systems, TPAs ensure accurate and consistent data tracking, providing a holistic view of employee health and plan performance.
- Claims Insights: TPAs can analyze claims data to uncover savings opportunities, ensuring that employers optimize their self-funded plans.
Looking Ahead: The Future of Self-Funded Health Plans with TPAs
The future of self-funded health plans is bright, with deeper integration of TPAs and an increasing emphasis onvalue-based care. As employers continue to demand greater transparency and efficiency in healthcare delivery, TPAs will evolve, leveraging advanced technology and data-driven insights to refine and personalize self-funded plans, as predicted byWoodruff Sawyer.
Continuous improvement will be essential to ensuring that these plans adapt to the changing needs of the workforce. TPAs will play a central role in driving these advancements, fostering a healthcare system that is both cost-effective and focused on the health and well-being of employees.
Conclusion:
Third-Party Administrators (TPAs) are revolutionizing the way self-funded health plans are managed. By taking on administrative tasks such as claims processing, cost management, compliance, and employee support, TPAs allow employers to focus on providing high-quality care to their workforce while reducing overall healthcare costs.
The integration of technology by using advanced tools to enhance the impact of TPAs, offering real-time analytics, predictive monitoring, and seamless integration with healthcare systems. For employers and healthcare professionals, embracing TPAs is not just a trend; it is a strategic step towards creating a smarter, more sustainable healthcare model that benefits both employers and employees.
Explore howHealth Compiler can elevate your self-funded health plan today and drive your healthcare strategy forward.
About Health Compiler:
Health Compiler is a healthcare analytics platform purpose-built to help employers, Direct Primary Care (DPC) practices, and value-based care teams turn complex healthcare data into clear, actionable insights. Founded by healthtech pioneers passionate about data interoperability and care transformation, Health Compiler integrates claims, EHR, labs, and pharmacy data into a unified view to drive better health and financial outcomes.
In addition to analytics, Health Compiler offers an AI-driven Practice Growth solution and AI Voice Call Triaging software, helping practices automate patient engagement, streamline administrative workflows, and grow more efficiently.
We are proud partners with Elation Health and Hint Health, and are HIPAA and SOC 2 compliant, ensuring the highest standards of security, privacy, and trust for all our customers.




